- Find a Provider
-
Services
-
Redeemer Health provides compassionate care across every stage of life.
- View all Services
- Health Care
- Cancer Care
- Heart Care
- Hospital at Home
- Maternity Care
- Pediatric Urgent Care
- More Health Care Services
-
- Patients & Visitors
- Locations
- Careers
categories:

If you’re a wartime veteran or the surviving spouse of a veteran who needs supportive care, you should know about a VA program that can help pay for that care.
The Aid and Attendance Pension, a benefit of the Department of Veterans Affairs, provides monthly income to veterans and their surviving spouses to help pay for an assisted living or personal care facility, home care provider, adult day center, or nursing home.
The program supports veterans who require care for a disability unrelated to their military service or need help with daily living activities. The VA will also provide income to a surviving spouse who was married to a veteran with qualifying military service. Eligibility is based on the veteran’s wartime service, health and care needs, income versus medical expenses, and total assets. In 2023, benefit will pay $1,432-$2,642 per month, tax-free.
A free webinar about the benefit, sponsored by Redeemer Health, took place on November 10, led by Emily Schwarz, President of AidandAttendance.com. You can view a video of the webinar here.
“A lot of veterans and surviving spouses don’t realize this program is available to help pay for assistance with care and activities of daily living,” says David McDonald, Personal Care Administrator for Redeemer Health. He notes that Redeemer Health offers two communities—in Northeast Philadelphia and Montgomery County—that accept the payments.
Who is Eligible?
AidandAttendance.com provides a short, free evaluation tool you can use to see if you meet eligibility criteria and are a good candidate to apply. More information on criteria and applying for the benefit are available at AidandAttendance.com.
Qualifying wartime military service includes:
- World War II
- The Korean Conflict
- Vietnam Era
- Gulf War
Types of care expenses that qualify include:
- Assisted living or personal care
- Home care
- Senior living (with care)
- Memory care
- Adult day care
- Nursing home
More information on the program is available by calling AidandAttendance.com at 800-626-7145 or the VA at 800-827-1000.
A Local Opportunity
Redeemer Health’s communities for older adults are among the facilities that qualify to accept the VA Aid and Attendance benefit. These communities help older adults stay safe and independent while enjoying access to therapeutic, social, recreational, and spiritual life opportunities.
Redeemer Health Lafayette in Northeast Philadelphia, and St. Joseph Manor in Meadowbrook, PA, offer personal care accommodations and services that include:
- A wide range of personal care apartments, suites, and rooms to suit many preferences and budgets
- Housekeeping and linen services
- Three meals daily
- Recreational programs
- Pastoral care
- Nightly check-in by nursing staff
- Assistance with medical appointment scheduling, medication management, dressing, washing and grooming
If residents' care needs should increase, the communities offer additional assistance via progressive levels of personal care.
Residents enjoy additional peace of mind knowing that the facilities' unique status as members of the Redeemer Health family gives them access to Redeemer Health's wide-ranging expertise and resources.
For more information on Redeemer Health's communities, visit redeemerhealth.org/lifecare/personal-care or call 215-214-2877.
categories:
I Believe in Hope
After Rosemarie Sulock's son was shot in the thigh while on duty as a Philadelphia police officer, she quickly lost 25 pounds. She thought it was due to stress.
Then her son's friend visited and, shocked by how thin Rosemarie looked, asked whether she had cancer.
Rosemarie thought about that conversation when she visited her gynecologist. Soon after, she noticed a round, stone-like object in her chest wall and, because she "knew her body," she asked for a mammogram.
She scheduled her mammogram with Anna Mazor, DO, breast surgeon with Redeemer Health in partnership with MD Anderson Cancer Center at Cooper. Dr. Mazor also performed an ultrasound.
Rosemarie said Dr. Mazor's pleasant demeanor put her at ease. "I just felt connected to her right away," Rosemarie said. "I felt like she was a friend I hadn't seen in a couple of years."
The ultrasound detected the object Rosemarie had noticed. Dr. Mazor immediately removed the small mass and used a fine needle to check for cancer cells.
Test results showed that Rosemarie had invasive ductal carcinoma, a type of breast cancer. Dr. Mazor recommended that Rosemarie have a lumpectomy, rather than a mastectomy, because they caught the cancer early.
As Rosemarie considered what to do, she mulled opinions from family members. She also was concerned about the timing, with her daughter's wedding coming up in a few months.
"I needed peace in my heart," Rosemarie said. So she went to the Healing Consciousness Foundation, a Redeemer Health affiliation which helps people affected by breast cancer improve their quality of life through education, lifestyle modification, and holistic healing.
Rosemarie chose to have the lumpectomy. During the procedure, Dr. Mazor also removed three lymph nodes. One turned out to be cancerous.
After her lumpectomy, Rosemarie needed radiation treatment. Under the care of radiation oncologist Sheena K. Jain, MD, Rosemarie received 32 radiation sessions. Still working, she traveled to her appointments during her lunch breaks.
Rosemarie finished treatment on Oct. 10, 2019 - "the happiest day of my life," she said. Following patient tradition, she rang a bell, which signified the end of her cancer treatment. Afterward, she ordered pizzas, hoagies "and all kinds of goodies" for the staff and gave them cards thanking them for pulling her through her cancer treatment.
"They were just so compassionate, patient, and loving," she said.
 She had a little time to recuperate before flying to Arizona for her daughter's November wedding. When she returned home, Rosemarie had contracted lymphedema, a non-lethal, but painful side-effect that some patients experience after cancer treatment. She had swelling and cording down her arm, which made her arm difficult to move. Dr. Mazor started her on eight months of physical therapy, including exercises Rosemarie did at home.
She had a little time to recuperate before flying to Arizona for her daughter's November wedding. When she returned home, Rosemarie had contracted lymphedema, a non-lethal, but painful side-effect that some patients experience after cancer treatment. She had swelling and cording down her arm, which made her arm difficult to move. Dr. Mazor started her on eight months of physical therapy, including exercises Rosemarie did at home.
Then in February 2020, Rosemarie learned that her breast cancer had returned. Out of caution, she sought a second opinion from another doctor, who confirmed Dr. Mazor's diagnosis of invasive mammary tubular carcinoma. Rosemarie returned to Dr. Mazor for another lumpectomy.
"I just love Dr. Anna," Rosemarie said.
Rosemarie noted that the receptionists at the doctors' offices were helpful. She also singled out for praise the nurse navigators in Dr. Mazor's office, who would call to check on her every few days. "Sometimes I cried on the phone with them," Rosemarie said. "I said, 'I feel like you guys are my family.'"
After the second surgery, Rosemarie underwent 21 radiation sessions. Unlike her first round of radiation, this time Rosemarie couldn't bring family or friends with her because of the COVID-19 pandemic. Staff kept her company, inquiring about her six grandchildren, including two sets of twins, and asking about the details of her daughter's wedding the previous year.
Today, Rosemarie is doing well. She now routinely sees hematologist and oncologist Pallav K. Mehta, MD for follow up care. She expects to see him for 10 years.
Rosemarie has gained back the weight she lost. In April, she turned 61. That same month, she had another mammogram. "Everything is clear," she said.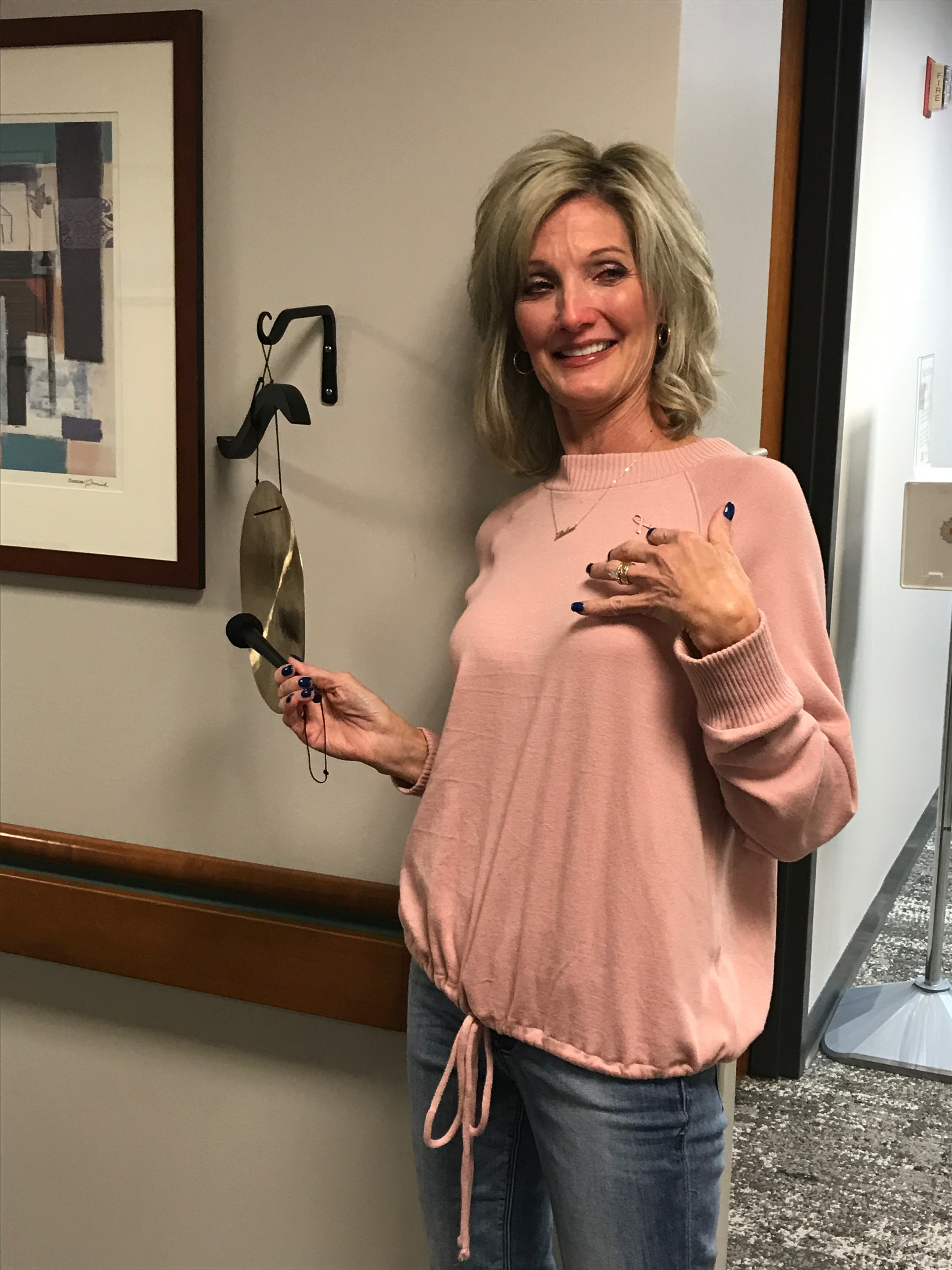
Rosemarie couldn't thank doctors and staff enough for their dedication and kindness, and for helping her to stay strong throughout her treatments.
"I believe in hope," she said. "I know the doctors at Redeemer Health in partnership with MD Anderson at Cooper all made me feel hope, and I continue to have hope for all those who are now going through cancer treatment."
Learn more about breast cancer services at Redeemer Health in partnership with
MD Anderson at Cooper.
categories:

We spend a great deal of time in our homes, especially so in the last two and a half years. While we consider our home a safe space, it is not without its fair share of risk, especially for seniors. According to the National Institute on Aging, six out of every 10 falls happen in the home. With September being Falls Prevention Month, here are some tips that you can use to easily fall-proof your home.
Avoid Clutter
First and foremost, keep hallways and stairs clear of any kind of clutter. Avoid keeping papers, clothes, books, and shoes in these areas as they present hazards. Keep electrical wires and cords away from these areas, as well. Wire covers or cable staples could assist with this by fastening the wires to an area of the wall and out of the way of walking paths.
Furniture can also present fall hazards, so ensure your furniture is organized efficiently and out of the way of any walking areas. Also, keep a close eye on your pets and where they are walking. Dogs and cats, no matter the size, could easily become tripping hazards.
Lighten Up Your Home
Lights throughout your home are critical for you to see any potential hazards. Consider having light switches at the top and bottom of stairs, as well as at both ends of hallways. Night lights in both your bedroom and bathroom provide additional support, especially during the evening hours.
Having a flashlight on hand by your bed is also crucial in case the power ever goes out in your home. Of course, just having these lights in place isn’t enough. Be sure to use them to avoid any potential falls.
Other Tools to Help Prevent Falls
There are several other tools that can help prevent falls, especially for use in the bathroom, which is the most dangerous room in your home for falls. Consider installing grab bars in showers and alongside the toilet, in addition to a raised toilet seat with handles. Tub/shower seats will also aid in preventing falls. Non-slip mats should also be used in your bathrooms, in addition to non-skid mats and strips throughout the other rooms of your home.
Consult with your primary care physician on whether or not canes or walkers would be beneficial for you. These devices help promote both safety and independence. An occupational therapy or physical therapy program could also be recommended. These programs improve and restore mobility, movement, strength, flexibility, balance, and coordination.
Did you know that Redeemer Health Home Care offers a fall risk home assessment program called Life Assess? Through this program a nurse visits your home to assess hazards within your home. We:
- Recommend simple home modifications to reduce risks of falls, like removing tripping hazards.
- Assess medications and blood pressure that may be causing falls or imbalance issues.
- Provide exercises to improve balance and strength.
- Provide strategies to address low vision.
- Provide strategies to help reduce falls at night and in the bathroom.
- Recommend any needed equipment and footwear to keep you safe in the home.
If you have questions about Redeemer Health Home Care, please visit our website, redeemerhealth.org/homecare, or call 888-678-8678.
categories:

Walking is one of the most accessible forms of exercise. Other than a sturdy pair of sneakers, you don’t need any special equipment, and the activity offers a multitude of health benefits. Plus, it’s free!
“Walking is such good exercise for most people because it is our most basic form of transporting the body,” says exercise physiologist Robert Catalini, manager of the Health and Fitness Center and Pediatric Rehabilitation at Redeemer Health.
Before starting on a walking regimen, Catalini says, people with conditions such as heart disease, hypertension, diabetes, or a history of stroke should get an all-clear from their doctor. And those who aren’t used to exercise should start gradually, perhaps with a five-minute stroll to the end of their block and back. Then go a little farther the next day. “Gradually increase your time,” Catalini says. “There’s no rush. Getting some form of exercise is better than nothing at all.”
Need incentive to get moving? Consider the following benefits.
- Trim excess inches: Being overweight can predispose you to other health issues. Walking a mile—which takes 15 to 30 minutes—burns about 100 calories. That means if you walked a mile every day, you would burn 36,500 calories in a year, which translates to losing 10 pounds. Plus, studies have found that walking reduces cravings for sugary foods.
- Improve heart health: A brisk daily walk elevates your heart rate and reduces your risk of problems such as high blood pressure, high cholesterol, heart attack, and stroke. Walking daily has been shown to reduce the risk of heart disease by 30 to 50%, but walking even a few times a week reduces that risk by 15 to 20%.
- Lower blood sugar: When you walk, your muscles use more glucose, the sugar in your bloodstream. Over time, this can lower your blood sugar levels. It also allows insulin to be used more effectively.
- Boost your mood: Joggers talk about the “runner’s high,” but you also can get a psychological boost from moving at a slower pace. Walking is reported to increase happiness and reduce anxiety, and a 2019 study published in JAMA Psychiatry found that walking for an hour a day can reduce your risk of major depression.
- Add years to your life: Walking is linked to a longer lifespan. A major study published in 2020 in JAMA found that the more steps participants over age 40 took, the lower their risk of dying from any causes. Taking into account subjects’ health, researchers found a 51% lower mortality risk for those who took 8,000 steps a day compared with those who took 4,000.
Walking is also known to reduce pain and boost your immune system. "The exercise is like medicine," Catalini says.
He encourages individuals to come up with a walking program to suit their physical condition, schedule, and lifestyle. "If it doesn't fit your lifestyle, you're not going to continue it," he says. "Your walking program becomes part of your lifestyle by being part of your routine."
Having a walking buddy or belonging to a walking group can help get you out the door. “If you have friends or neighbors that you can say, ‘Hey let’s go for a walk,’ I think that’s a great thing to do,” Catalini says. “Now it becomes a social thing as well as a physical thing.”
Walkers also can get their steps in while supporting a worthy cause at events such as the fundraising walks Redeemer Health will hold this fall at Bryn Athyn College. The Kohl's + Redeemer Health NICU 6K Walk /Run on September 24 will support Redeemer’s Neonatal Intensive Care Unit. The Hope is Here: 2022 Breast Cancer Awareness Walk on October 15 will support the breast health programs at Redeemer Health in partnership with MD Anderson Cancer Center at Cooper.
Wherever and whenever you elect to walk, Catalini offers the following tips to help ensure a safe and positive experience:
- Invest in proper footwear. The professionals at your local running store should be able to help.
- Consider walking indoors, on a treadmill or at a mall, during inclement weather.
- Avoid walking in the middle of the day in the summer, when it tends to be hottest.
- Be sure to hydrate.
Now all that's left is to take the first step.
categories:

Pregnant with twins, Cassandra first noticed pain in her right shoulder about 27 weeks into her pregnancy. The pain subsided, but within a few weeks the pain returned even stronger.
The extreme pain led Cassandra to Holy Redeemer’s Labor and Delivery Unit, where we diagnosed her with a form of pre-eclampsia known as HELLP (Hemolysis, Elevated Liver Enzymes and Low Platelets).
Cassandra’s platelet levels were going down and her liver function was failing. She remembers the caring hospital staff doing everything they could. “They tried as much as possible to prolong the pregnancy, but it just wasn’t going to happen,” she said.
Cassandra’s twins were born at 29 weeks and a day—about 11 weeks premature. Logan weighed 2 pounds, 15 ounces. And Michael was just 2 pounds, 6.7 ounces.
Logan was intubated and sent immediately to Holy Redeemer’s Neonatal Intensive Care Unit (NICU). Michael was placed on continuous positive airway pressure (CPAP) therapy and transported to the NICU, where he was eventually intubated.
For every precious baby we welcome into the world, it's our mission to send them home as safe, healthy, and as fast as possible. For Logan and Michael that journey home took 62 days in our NICU.
Looking back, Cassandra feels a roller coaster of emotions, but only positive memories of the exceptional care the boys received while in the Holy Redeemer NICU. The doctors and nurses became like family to both her and her husband, providing their boys both compassionate and state-of-the-art care.
Part of the care Cassandra is especially grateful for are the “giraffe beds” both boys stayed in during in their first few weeks of life. The beds are designed to model a mother’s womb as it relates to things like temperature and humidity--keeping premature babies warm, keeping their delicate skin in good condition, and allowing them to grow in an optimal place.
Since Cassandra was recovering from a C-section, the beds could adjust so she was able to see and touch the boys with ease.
“Because I was recovering from a traumatic delivery, staff were able to lower the bed, so I was eye-to-eye with the boys. I could reach in the side to take part in their care even though I couldn’t stand at the time. That meant the world to me,” Cassandra said.
The beds also raised and lowered to allow the NICU staff to monitor, weigh, and even X-ray the boys without having to remove them from their beds. Keeping them in place reduced their risk of complications from environmental changes.
Plus, as Cassandra notes, it kept from having to disturb them. “At 29 weeks, every little bit of energy they have to expend is huge, so not having to expend that energy moving was important for them,” she adds.
Today, the twins are nearly seven months old and healthy and happy at home with mom and dad. And Cassandra is grateful for those who have contributed to make giraffe beds possible at Holy Redeemer Hospital, as she knows those beds made their difficult journey that much easier.
Now the Redeemer Health community is coming together to fund an additional Giraffe Omnibed Carestation for our NICU. Funds raised from our upcoming Kohl’s + Redeemer Health 6K Run/Walk on September 24th will help. We invite you to register or donate today by visiting runsignup.com/gotheextramile.
categories:

(Philadelphia, PA) – An alliance composed of Temple Health, Redeemer Health, and Philadelphia College of Osteopathic Medicine (PCOM) has signed a definitive agreement whereby a newly formed entity owned by the Alliance will acquire Chestnut Hill Hospital as part of an asset purchase transaction with Reading, PA-based Tower Health pending review and approval by regulators and the Tower Health bond holders.
“Together, our organizations bring the expertise, resources, operational excellence and skilled clinical care to ensure that Chestnut Hill Hospital remains a durable and sustainable resource for the eastern Montgomery County and northwest Philadelphia communities,” said Michael A. Young, MHA, FACHE, President & CEO of Temple Health. Temple Health will manage the newly-named Temple Health-Chestnut Hill Hospital following the acquisition.
Temple Health, Redeemer Health, and PCOM formed the Alliance to pursue collaborative affiliations that will benefit patients and add value to the communities they serve. “Our collaborative affiliation promises continued success for our organizations and those we partner with, and more importantly, for the patients and communities we serve,” said Michael B. Laign, President & CEO of Redeemer Health.
“This endeavor will help strengthen PCOM’s clinical and graduate medical education capabilities and enhance our ability to train the next generation of health professionals,” said Jay S. Feldstein, DO, President and CEO of Philadelphia College of Osteopathic Medicine. “Most importantly, Chestnut Hill Hospital will continue to serve as a critical resource for the surrounding communities.” Chestnut Hill Hospital has served the northwest Philadelphia and east Montgomery County area for more than 100 years.
“Tower Health is pleased and grateful that Chestnut Hill Hospital will continue to serve the community as part of an alliance of highly-respected and locally-based non-profit healthcare institutions,” said Tower Health President and CEO P. Sue Perrotty.
