- Find a Provider
-
Services
-
Redeemer Health provides compassionate care across every stage of life.
- View all Services
- Health Care
- Cancer Care
- Heart Care
- Hospital at Home
- Maternity Care
- Pediatric Urgent Care
- More Health Care Services
-
- Patients & Visitors
- Locations
- Careers
categories:

Maintaining a healthy lifestyle is important when you are planning your pregnancy. Consider the following while trying to conceive:
Schedule a visit to your OB/GYN prior to conception to discuss any questions or concerns you or your partner might have and get recommendations on how to optimize your health prior to becoming pregnant.
Maintain a healthy weight. If you are a normal weight before pregnancy, gaining 25 to 35 pounds during pregnancy is advisable. If you are underweight prior to pregnancy, you should gain enough to be within a normal range. Excess weight prior and during pregnancy increases your risk of several conditions that can negatively impact you and your baby.
Start taking prenatal vitamins with folic acid at least 1 month before pregnancy and continue through your pregnancy. Because folic acid is important for your baby’s development and getting enough is difficult through diet alone, taking a vitamin supplement is recommended. Consider talking to a nutritionist about your diet to incorporate the nutrients needed for your baby’s prenatal development.
Stop smoking, drinking alcohol and recreational drug use, these substances can have very harmful effects on your baby, especially in the first trimester. Your doctor can help create a plan to taper off of these substances before trying to conceive.
Prior to conception, monitor any special medical conditions that you might have such as high blood pressure, diabetes, depression, or seizures. It is important to manage these conditions. Do not stop prescribed medication. Talk to your doctor about the medications you are currently taking, including over-the-counter and natural medications. Some medications might not be safe during pregnancy.
Be prepared to provide your physician with a thorough medical history for you, your partner and both of your families. Some conditions are inherited, and you may want to consider genetic testing prior to pregnancy to make sure you have the best chance of having a healthy baby.
Planning ahead before getting pregnant can make a big difference during your pregnancy for both you and your baby. These tips can help you get started; but be sure to ask your doctor what would be best for you.
To find an OB/GYN that’s the right fit for you check out our Redeemer Health providers.
Dr. Jessica Kroes from Women’s Care is here to help patients with their journey. “When someone comes to the doctor, they might be nervous, they might be vulnerable if it is there first pregnancy, and they may have a lot of questions. Listening to the patients and being their support is extremely important.”

Meet Jessica
Dr. Kroes specializes in Obstetrics & Gynecology with our Women’s Care Center. She has a degree from La Pontificia Universidad Javeriana, and completed her residency at the Bronx Lebanon Hospital Program associated with Mount Sinai. Her passion for OB/GYN is driven by the lifetime bonds she builds with her patients. When she’s not sharing baby talk, Jessica enjoys traveling, playing tennis and cooking. She’s fully bilingual in Spanish and English.
categories:
Cancer of the colon or rectum is the second leading cause of death from cancer in the U.S. But the outlook is bright: Experts are studying ways to prevent this cancer that attacks the digestive system.
Six Lifelong Habits
Research shows that the following tactics can lower your risk for colon cancer:
- Maintain a healthy weight and participate in regular physical activity.
- Limit your intake of red meat and animal fats
- Eat a diet high in fruits, vegetables and whole grains
- Curb your alcohol consumption. Also quit (or never start) smoking cigarettes.
- Increasing the amount of folic acid and vitamin B-6 in your diet may offer protection against colon cancer. However, supplementing with vitamins containing folic acid or B-6 does not appear to provide protection.
- Get adequate calcium and vitamin D from foods or a supplement. Talk with your doctor about calcium amount recommendations as there are several conditions where calcium supplementation can be dangerous.
The Seventh Strategy: Screenings
“Most curable colon cancers occur in patients who did not have symptoms at the time of diagnosis,” says Dr. Soo Kim, colon and rectal surgeon with Colon and Rectal Associates, Ltd. at Holy Redeemer. “Even if you have no symptoms whatsoever, that colon cancer screening is a MUST.”
Colon cancer may cause symptoms including:
- Blood in the stool
- Recurrent stomach pain or cramping
- Stools narrower than usual
- Unexplained weight loss
The American Cancer Society recommends people with an average risk for colorectal cancer start regular screening at age 45, while the U.S. Preventive Services Task Force advises beginning screening at age 50. If you have an increased risk for colorectal cancer, you may need to get tested at an earlier age. People at increased risk include:
- Individuals with a personal or family history of colon cancer or polyps, which are precancerous growths in the colon or rectum
- Anyone with inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease.
To learn more or to schedule a colonoscopy or call 215-517-1250.
categories:

Myth: You have to drink milk to make milk
Fact: You do not need to drink milk to make milk. Your body works on the simple principal of supply and demand, or really demand and supply. When the baby takes the milk out, the body replenishes. The more you nurse or pump the more milk your body will produce.
Myth: You don’t have enough milk until day three when your milk comes in
Fact: Trust your body. Trust the process. Your first milk, called colostrum, is produced in a limited quantity, but it’s perfectly balanced for baby’s belly.
Myth: The first milk colostrum is all baby needs. You don’t need to breastfeed longer than a few days
Fact: Breastmilk contains vital cells that fight off bacteria and viruses while you nurse. Also, breastfeeding has many other important health benefits for your baby. The American Academy of Pediatrics recommends that infants be exclusively breastfed for about the first 6 months with continued breastfeeding along with introducing appropriate complementary foods for 1 year or longer.
Myth: If baby nurses longer than 15 minutes, you’re their pacifier
Fact: Babies breastfeed for more than milk. They come for thirst, hunger, love and comfort. Sucking is a positive response and promotes milk production.
Myth: Feeding on demand creates a demanding child
Fact: Feeding your baby when they’re hungry and holding them when they’re upset is precisely what mom should do. The number of feedings your baby needs each day depends on your milk storage capacity. A mother with a large storage capacity can feed her baby less times each day. Your baby will let you know how much they need. Remember, watch for feeding cues!
Myth: Women with small or large breasts don’t make enough milk
Fact: Your breast size doesn’t come into play when it comes to milk production, even though they do get bigger once baby comes! Fatty tissue determines breast size. Milk is made in the ducts, not from the fatty tissue.
Myth: Breastfeeding always hurts
Fact: In the first two weeks, you may feel some pain in the first 30 seconds of feeding. If you’re experiencing more, your latch should be checked by a lactation consultant. Sometimes simple adjustments to latch and positioning can eliminate pain.
Myth: Eating gassy foods gives your baby gas
Fact: Your breast milk is made from your blood. We get gas when we try to digest the fiber in food like broccoli and cabbage. Since your baby doesn’t ingest the fiber, they won’t experience the gas from those foods. Babies can be gassy, but don’t blame the beans. And remember, the healthiest foods for us are often the gas producers.
Got more myths we can help bust or any advice / feedback on breastfeeding to share? Post any questions or comments you may have below.
To speak with or to schedule an appointment with a lactation consultant, reach out to the Breastfeeding Resource Center.
categories:

It’s a sensitive subject. But it needn’t be. We’re here to talk about it all. Because it’s time pelvic floor wasn’t taboo. We’re here to share the all natural nitty gritty, about your pelvic floor. And more. Maybe you haven’t really thought why your pelvic floor matters. As a web of muscles, ligaments and tissues that stretches across your pelvic bones, it does the important job of supporting all your pelvic organs. These organs include your vagina, womb, bladder and bowels.
During pregnancy our core, which includes your pelvic floor, back, abdomen, and hips, undergoes a lot to nurture your little bundle of joy. Over nine months and during birth, the muscles in your pelvic floor become stretched. The weight of your baby, hormones that loosen your tissues, and the efforts of labor all put extra pressure on this part of your body. As a result your pelvic floor may become weakened or damaged. This isn’t unusual. In fact, many moms experience changes after pregnancy.
Don’t suffer in silence
This means you may experience leakage or gas when you exert insignificant levels of energy. For instance some women experience leakage when lifting their baby, grabbing groceries, coughing and sneezing-- or even laughing! Some women also suffer from back, hip, and pelvic floor pain. But this condition isn’t irreversible. You don't have to suffer in silence. And no, you don’t have to laugh it off. Because many moms are finding yoga is a successful way to improve postpartum pain, leakage, and postural changes.
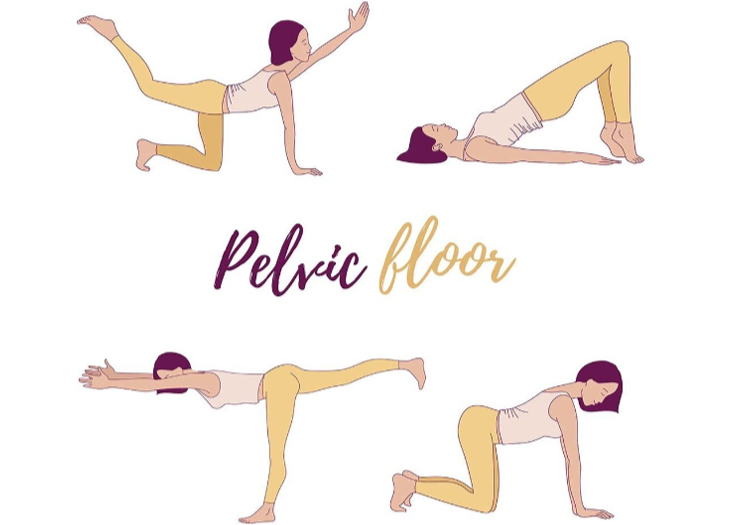
These common yoga moves may be helpful to try at home in the postpartum period:
Let’s customize a personal core program
However, not all exercises are optimal for everyone. So you may want to consider consulting a female therapist who specializes in pelvic floor and women’s health. Sharing details with an expert may feel intimidating, but as with your obstetrician, you’ll quickly develop a comfort level and rapport. By assessing your personal needs and developing a personal program of exercises and manual therapy, you can partner on improving your symptoms together.
Redeemer Health offers this type of discrete specialized care. If you think you would benefit from pelvic floor/ women's health physical therapy, please call 215-938-5621
Has pelvic floor therapy or yoga helped you? We’d love to hear your experience in the comments below.
categories:

On February 1st, the Thursday before the Super Bowl, the Holy Redeemer Maternity Unit, was popping with Philadelphia Eagles pride. Babies donned their custom hats. Nurses flaunted their favorite Eagles gear. And pennants reminded visitors of last year’s champs. All in celebration of the Eagles’ tinniest fans.
Busy hands. Happy hearts
Thanks to the creative energies of Marie Milcarsky and Dorothy “Dot” McHale no head was ignored. Because every baby in the NICU and Maternity Unit received a special handmade Eagles hat to wear for the big game.
Marie, a housekeeper with Holy Redeemer Hospital, has crocheted miles of yarn in her time. Making baby hats for the past seven years, she’s hooked creations for every occasion. Even an impressive white crown for the first baby born in 2018. Meanwhile fellow maker Dot, an 80-year-old retired resident of Maple Shade, NJ, thought it would be fun to make red baby hats to honor February’s heart month theme. But she didn’t stop there. After watching tutorials on YouTube, she got the idea to make the babies green football hats in honor of the Super Bowl.
Yarn: the healer
Dot, accompanied by her daughter, Maureen, a Redeemer Health employee, attended our Tiniest Fans Pep Rally and hand delivered her precious hats to the tiniest fans. Clearly Dot and Marie know they like to crochet. But what they may not know is that several health authorities agree about handicraft. It’s believed that using knitting or crochet as meditation can be a daily way to minimize the effects of stress in your life. Which ultimately can help reduce heart disease.
Hooking or knitting is also a great way to build a community and reduce depression and isolation. So maybe it’s time for us all to consult YouTube and start making.
Game on
The Tiniest Fans Pep Rally gathered over 40 Eagles fans ready to cheer on the Birds in the big game. Staff, employees, proud parents and picturesque hat- wearing babies all showed up. The tiny pep rally also drew attention from local news outlets including Fox29, 6ABC, NBC10, CBS3, and the Bucks County Courier Times.
categories:

When you’re pregnant many doctors provide a long list of foods and beverages that are off limits. We know this can feel restrictive. But, thankfully there’s a much longer list of appetizing things you can enjoy. These foods help support a healthy pregnancy, keep you feeling well, and help your baby thrive.
With the extra demands on a woman's body and the increase in blood volume, anemia is a very common condition in pregnancy. In fact, about one of every two pregnant women doesn’t get enough iron. Low levels can increase your risk for preterm birth of low birth weight. You may feel tired, weak, or dizzy, or experience headaches if your iron levels are too low.
Pumping iron
Iron is found in many foods including dark, leafy greens, such as broccoli, brussel sprouts, spinach, collard greens and kale. It’s also found in dried fruits, fortified cereals and grains. Meat (particularly red), fish and tofu are a great source of iron. As are lentils, peas and beans. Integrating extra iron into your diet can be as simple as adding dried apricots or figs to your store-bought cereal or trail mix. Consider replacing that iceberg side salad with some dark leafy greens like baby kale or arugula. Or try roasted brussel sprouts as a healthy side. Thinking about adding extra iron to every meal can take a little practice. But, once you get creative, you’ll reach your daily recommended dose of 27 milligrams of iron in no time.
Try this family friendly broccoli frittata
Cooking when you’re tired can be exhausting. We get it that mommy-to-be needs all the help she can get. So here’s a super healthy meal the whole family will like. With 15% of your daily recommended iron intake it’s a smart, and easy choice...
1/2 cup nonfat cottage cheese
2 cups fat-free egg substitute
1 large onion, diced
1 tsp. olive oil
2 cups frozen chopped broccoli
1/2 tsp. dried dill
2 tsp. margarine
Mix cottage cheese and egg substitute together, set aside. In large nonstick frying pan over medium heat, saute onion in oil for five minutes, or until soft. Add broccoli and dill; saute for five minutes, or until the mixture softens. Set aside.
Wipe out frying pan. Add 1 tsp. margarine and swirl the pan to distribute.
Add half of the vegetable mixture, and then half of the egg mixture; lift and rotate pan so that eggs are evenly distributed. As eggs set around the edges, lift them to allow uncooked portions to flow underneath. Turn heat to low, cover the pan, and cook until top is set. Invert onto a serving plate and cut into wedges. Repeat with remaining 1 tsp. margarine, vegetable mixture, and egg mixture. And that’s it!
Serves 4: Each serving provides: Calories 150, Total fat 3 g, Saturated fat 0 g, Cholesterol 0 mg, Sodium 390 mg, Total carbohydrate 12 g, Fiber 3 g, Sugar 3 g, Protein 19 g.
Got an iron-rich recipe you really like? Share it with all of our moms in the comments section below!
categories:

Welcome to the third trimester! As the time approaches to meeting your little one, you may be wondering what you should be doing during the last part of your pregnancy. Here is a list of ten things for your to-do list in the third trimester:
1. Get Familiar with Third Trimester Screenings and Visits
The frequency of your routine check-ups will increase during the last trimester to every two weeks, and eventually every week. Your doctor will want to perform certain tests, such as Group B Strep, and administer any immunizations you may want. If your blood type is Rh Negative, you will most likely receive a Rhogam injection, if you haven’t had one already during your pregnancy. Ask your doctor for a list of tests and additional exams you can expect in your third trimester.
2. Finish Taking Prenatal Classes
Take a look at all of the classes offered in your area, and decide which ones would benefit you. Remember to sign up as early as possible, as these classes can fill up quickly. Consider classes such as childbirth, breastfeeding, or infant CPR. Here’s a link to classes offered by Redeemer Health.
3. Start Doing Kick Counts
Around week 28, start keeping track of your baby’s movements. The general rule of thumb is ten fetal movements in two hours. If you notice any decrease in movement, it’s a good idea to notify your doctor.
4. Choose a Pediatrician
Before you go into labor, you should choose a pediatrician for your baby. Doctor’s offices will typically hold meet and greet sessions, where you can familiarize yourself with the staff and the office policies.
5. Read and Ask Questions about Breastfeeding
If you have decided to breastfeed your baby, now is the time to learn about what to expect and any complications that may arise. It’s often a good idea to take a breastfeeding class if this is your first baby. The key to breastfeeding successfully and in a way that’s healthy for you and baby is having the support YOU need. The Breastfeeding Resource Center is here to help.
6. Take a Hospital Tour
Before going into labor, try to take a tour of the hospital or birthing center where you intend to give birth. This gives you the opportunity to get familiar with the layout of the facility.
7. Install the Car Seat
All babies are required to ride home from the hospital in a car seat, and now is a good time to have it installed. Often, you can take the car seat to a local fire or police department certified in car seat installation, and have them install it for you to make sure it is done correctly.
8. Read and/or Take a Class on How to Take Care of Baby
Now that you’ve probably read all about your pregnancy, it’s time to start reading about how to care for your baby once they arrive. Redeemer Health offers a few options for classes.
9. Know the Signs of Labor
There are several signs your body is preparing for labor, including regular tightening in the pelvic area and the onset of a backache. Knowing the signs that you might be in labor is important so you know when to call your doctor and when to head to the hospital. Experiencing any of these signs before 37 weeks could indicate preterm labor, and should be reported to your doctor right away.
10. Plan or Plans in Place For When You Go Into Labor
As soon as your contractions begin, you will want to have a plan in place so you know who you should call and where you need to go. Have your hospital bag ready so you will have one less thing to worry about before heading out to meet your baby.
While it seems like there’s a lot to do before baby comes, the third trimester is also a good time to slow down, relax and enjoy the final stage of your pregnancy. The best is yet to come!
categories:
Hearing that a loved one will benefit from hospice care may result in a flood of emotions.
Perhaps the news that a loved one has a limited life expectancy was unforeseen and a departure from the hope for a cure that once occupied your thoughts. Perhaps the suggestion of hospice care comes as a relief and provides hope that help will soon be available to provide much needed comfort, support, and care coordination.
Whatever the circumstance that leads to a recommendation for hospice there may be many questions that follow. What is hospice care? How can they help me and my loved one? And how do I choose a hospice? You may find that there are just a few hospice programs in your region, or you may find as many as 80 or more hospices to choose from.
The following questions may guide you in knowing what to ask and help you in making an informed decision when choosing a hospice provider:
Is the hospice program certified and licensed by the state or federal government?
Most hospices are certified by Medicare and licensed by the state where they provide care. This ensures that certain rules are followed, required services are provided, and that Medicare or Medicaid will pay for services.
What other kinds of accreditation or certification does the hospice program or its staff have?
While not required, many hospices seek accreditation from national organizations that ensure the hospice meets quality standards. Also, hospice team members may have certification in hospice and palliative care or in their profession.
Can I get references, or find out about any accreditation a hospice has?
Yes. The National Hospice and Palliative Care Organization maintains a directory of all organizational members, providing information about certification and accreditation status as well as other important program information.
How long has the hospice been servicing your community? Who owns or governs the hospice?
How long a hospice has serviced your community, and whether a hospice is not-for-profit, for-profit, faith-based, free-standing, or part of a health system may be important to you.
What screening and training do staff and volunteers receive?
Ask about the number of hours and content of initial training as well as the hospice program requirements for ongoing education of staff and volunteers.
What additional services or programs does the hospice offer?
Federal regulations require all hospices to provide nursing, social work, pastoral care, hospice aide, volunteer, and certain bereavement services. Some hospices have additional services that may include complementary therapies, community bereavement programs and support groups, palliative care, veterans’ programs, pediatric care, or specialized volunteer programs, to name a few.
How does the hospice respond to calls and concerns in the evening, night, and weekend hours?
Ensuring that help is available to you at any time of the day or night to address your concerns and visit your home, when necessary, is critical. Find out how the hospice will respond to these needs.
What will happen if the care can’t be managed at home?
While the needs of nearly all people can be managed in the home, knowing what other options are available for assistance in the event of medical crisis will bring you much needed peace of mind. Some hospices have freestanding inpatient hospice units or houses, while others contract with local hospitals or nursing homes.
What measures does the hospice use to ensure quality?
Public quality reporting for hospice programs will begin within the next year. Many hospices are already collecting data regarding certain quality measures. Inquire about what measures the hospice collects, including how quickly pain and other symptoms are controlled and what actions the hospice has taken to improve in these areas.
Does the hospice measure family satisfaction with care?
Through a brief survey, many hospices ask family members for feedback about care in order to ensure excellence and improve where necessary. Ask the hospice if they measure family satisfaction and how their results compare to other programs.
It is increasingly common for healthcare consumers to explore options and even interview providers prior to making care decisions. Hospice is no exception. Whether choosing between three hospices or 80, understanding what makes hospice programs similar and understanding how they may be different is essential to choosing a hospice that will meet the unique needs of you and your loved one.
To learn more about hospice services at Holy Redeemer, visit Hospice Care.
